Santa Clarita Valley,
your healing starts here

At Santa Clarita Valley Wound Care and Hyperbarics, we utilize advanced procedures as well as hyperbaric oxygen therapy to focus on healing wounds that the body is struggling to heal on its own. With proper intervention and treatment, we can bring healing, oftentimes within eight weeks.
Services we provide
Wound Care
Our wound care specialists provide advanced procedures to promote healing, providing personalized care plans to address your unique wound care needs.
Wound healing in less than 8 weeks
Hyperbaric Oxygen Therapy
Our hyperbaric oxygen therapy is a non-invasive treatment that stimulates healing and fights infection, helping to heal wounds faster and more effectively.
Infection Prevention and Management
We specialize in infection prevention and management, providing comprehensive care to ensure that your wound stays clean and free from infection.
What is a Chronic Wound?
Wounds that are unable to heal on their own are considered chronic wounds. They occur for a number of reasons, ranging from diabetes to arterial diseases, and can be both painful and detrimental to your health. The sooner you seek the help of an experienced wound care team, the sooner we can get you back to living life.


What is Hyperbaric Oxygen Therapy?
Hyperbaric Oxygen Therapy (HBOT) is the administration of 100 percent oxygen in a safe, pressurized environment. The therapy works throughout your entire body as
the increased levels of oxygen enter the bloodstream and tissue to promote the healing of chronic wounds. The amount of time each treatment takes depends on the individual, usually lasting approximately two hours and given five days a week.
This non-invasive procedure can offer many benefits, including:
- Preservation of injured tissue
- Improve delivery of oxygen to injured tissue
- Improve wound healing
- Improve control of certain infections
- Improve growth of new blood vessels
Wounds We Treat
We treat all chronic, non-healing wounds but we specialize in treating the following types below.
Traumatic Wounds are defined as:
- Caused by External Force: These wounds occur due to an external physical impact, such as cuts, blunt force, or punctures.
- Tissue Damage: They involve damage to the skin, underlying tissues, muscles, and sometimes bones and internal organs.
- Acute in Nature: Traumatic wounds typically occur suddenly and can be either minor or severe, depending on the force and the part of the body affected.
- Varied Healing Times: Healing can range from quick recovery to requiring extensive medical intervention, depending on the wound’s depth, location, and the individual’s health.
Diabetic wounds are typically characterized by their chronic nature and difficulty in healing due to poor blood circulation and nerve damage associated with diabetes. Common features include:
- Slow Healing: Due to impaired blood flow and oxygen delivery to tissues.
- Infection Prone: High blood sugar levels can weaken the immune system, making wounds more susceptible to infections.
- Neuropathy: Reduced sensation in extremities can lead to unnoticed injuries.
- Ulcers: Particularly common on the feet (diabetic foot ulcers), resulting from pressure points and minor trauma.
- Ischemia: Reduced blood supply to the affected area, hindering healing.
- Calluses: Thickened skin around the wound edges due to repetitive stress.
- Drainage and Odor: Persistent drainage and sometimes a foul smell if infected.
- Gangrene Risk: Severe cases can lead to tissue death and possible amputation.
Effective management requires strict blood sugar control, proper wound care, and sometimes surgical intervention.
Venous Leg ulcers are chronic sores on the legs that fail to heal properly, often recurring due to venous insufficiency, diabetes, and other vascular diseases. They are characterized by:
- Persistent Open Wounds: Sores that do not heal within a few weeks.
- Pain and Discomfort: Varying from mild to severe.
- Swelling: Particularly around the ankle.
- Discoloration: Skin around the ulcer may appear darkened or reddish.
- Oozing: Possible discharge of fluid or pus.
- Crusting and Scabbing: Especially if the ulcer is infected or healing slowly.
- Itching and Irritation: Common symptoms that can lead to further skin damage if scratched.
- High Risk of Infection: Due to the open nature of the wound and its chronicity.
Effective treatment and management involve addressing underlying conditions, proper wound care, and sometimes medical interventions like compression therapy or surgery.
Arterial ulcers typically happen when blood is unable to flow into the lower extremities, like the legs and feet. When the skin and underlying tissue are deprived of oxygen, the tissue starts to die off and form an open wound.
Arterial wounds are most often caused by blocked arteries. This may prevent nutrient-rich blood from flowing to the extremities, creating an open wound and preventing wounds from closure.
Other potential causes include:
- Poor circulation
- Arteriosclerosis or atherosclerosis
- Venous insufficiency, when blood in your leg veins doesn’t flow back up to your heart
- Diabetes
- Kidney failure
- Hypertension (high blood pressure)
- Lying or sitting in one position for too long
- Other disorders may also lead to arterial wounds, including high cholesterol, heart disease/Peripheral Arterial Disease, high blood pressure, or sickle cell anemia.
While your body can heal arterial wounds on its own, the natural healing process will be significantly slower due to circulation issues. Many people with arterial ulcers experience chronic pain and sores that take months or years to fully heal without specialized intervention.
Acute arterial insufficiency results from a sudden interruption in blood flow to a particular area, caused by a blockage or severe narrowing of an artery.
- Sudden Onset: Symptoms appear rapidly due to the abrupt interruption of blood supply to tissues.
- Pain: Patients may experience severe, localized pain, often described as intense and disproportionate to physical findings.
- Pale Skin: The affected area may appear pale or blanched due to reduced blood flow.
- Coolness: The skin may feel cool to the touch as a result of diminished circulation.
- Delayed Capillary Refill: Capillary refill time is prolonged due to impaired blood flow.
- Muscle Weakness or Paralysis: In severe cases, muscle function may be compromised due to lack of oxygen and nutrients.
- Gangrene: Without prompt treatment, tissue death (gangrene) can occur, leading to serious complications or limb loss.
Early recognition of acute arterial insufficiency and intervention are crucial to prevent irreversible tissue damage and preserve limb function.
If you are experiencing acute arterial insufficiency contact your vascular surgeon/interventional radiologist/cardiologist immediately. If you are not under the care of a specialist, call 911 and go directly to the emergency department for care.
Pressure injury wounds, also known as bedsores or decubitus ulcers, are injuries to the skin and underlying tissue caused by prolonged pressure. They typically develop on bony areas such as the heels, ankles, hips, and tailbone. These injuries are classified by stages:
- Stage 1: Reddened, non-blanching skin that may be painful but intact.
- Stage 2: Partial-thickness skin loss with exposed dermis, presenting as an open blister or shallow ulcer.
- Stage 3: Full-thickness skin loss extending into the subcutaneous tissue, potentially exposing fat but not muscle, tendon, or bone.
- Stage 4: Full-thickness tissue loss with exposed muscle, tendon, or bone, often accompanied by tunneling or undermining.
- Unstageable: Obscured full-thickness skin and tissue loss. Can be difficult to confirm. If slough or eschar is removed, a Stage 3 or 4 pressure injury is revealed. Stable eschar on the heel or ischemic limb should not be removed.
- Deep Tissue Pressure Injury: Non-blanchable deep red, maroon, or purple discoloration. Intact or broken skin often with a dark wound bed or blood-filled blister. Pain and temperature changes usually precede discoloration. If necrotic, subcutaneous, granulation tissue or fascia are visible, this indicates a stage 3, 4 or unstageable.
Risk factors include immobility, poor nutrition, and moisture. Prevention involves regular repositioning, skin care, and using pressure-relieving devices. These wounds can lead to severe complications like infections and require comprehensive medical care.
Chronic non-healing wounds are persistent injuries that fail to progress through the normal stages of healing within an expected timeframe, typically over three months. They often exhibit continuous inflammation, poor blood circulation, and infection. These wounds can be characterized by the following:
- Prolonged Inflammation: Persistent redness, swelling, and pain.
- Poor Blood Flow: Insufficient oxygen and nutrient supply, common in diabetic ulcers or venous leg ulcers.
- Recurrent Infection: Frequent or persistent infections delaying healing.
- Necrotic Tissue: Presence of dead tissue, which hinders the healing process.
- Exudate: Excessive drainage or fluid from the wound.
- Edge Maceration: Surrounding skin may be softened or damaged due to prolonged moisture exposure.
- Lack of Granulation Tissue: Poor formation of new connective tissue and blood vessels.
Underlying Health Conditions: Often associated with diabetes, vascular diseases, obesity, or compromised immune systems.
Surgical wounds exhibit specific characteristics that distinguish them from other types of wounds. These wounds typically result from surgical procedures and are characterized by the following features:
- Clean Edges: Soft surgical wounds often have well-defined, clean edges due to precise incisions made during surgery.
- Minimal Trauma: Compared to traumatic wounds, soft surgical wounds involve minimal tissue damage, as they are intentionally created under controlled conditions.
- Controlled Bleeding: Surgical wounds are typically created with meticulous care to minimize bleeding, often with the use of cautery or sutures to control blood flow.
- Sterile Environment: Surgical wounds are created in a sterile environment to reduce the risk of infection, promoting optimal healing.
- Closure Method: Soft surgical wounds are commonly closed using sutures, staples, or adhesive strips to facilitate proper wound healing and minimize scarring.
- Postoperative Care: Proper postoperative care, including wound dressing changes and monitoring for signs of infection, is essential for the successful healing of soft surgical wounds.
Even when all the above measures are following some surgical wounds that are sutured closed (primary closure) may open (called dehiscence) and require healing via secondary intent. Our team of wound care specialists can guide the healing process of these wounds.
Secondary intention healing: Open wounds that heal from the base up via granulation followed by epithelialization. These wounds cannot be sutured closed (primary closure).
Post-Mohs procedure wounds exhibit specific characteristics due to the nature of Mohs micrographic surgery, a precise technique for removing skin cancer layers. These wounds are typically:
- Precise: Mohs surgery removes cancerous tissue layer by layer, aiming for maximal tumor removal while preserving healthy tissue.
- Variable Size: Wound size varies depending on the extent of cancerous tissue removed, ranging from small to large areas.
- Depth: The surgery may penetrate deep into the skin layers, necessitating careful wound management to promote healing.
- Irregular Shape: Wounds can have irregular shapes due to the selective removal of cancerous tissue, requiring tailored closure methods.
- Potential for Tension: Closure of larger wounds may require techniques like sutures or skin grafts to minimize tension and optimize healing.
- Risk of Complications: Due to the surgical depth and potential size, post-Mohs wounds are susceptible to infection, delayed healing, or scarring, necessitating close monitoring and appropriate wound care.
Chronic refractory osteomyelitis wounds are characterized by persistent inflammation and infection of bone tissue, often resistant to conventional treatment methods. These wounds typically exhibit the following features:
- Long-standing Infection: They result from untreated or inadequately treated acute osteomyelitis, leading to chronicity.
- Recurrent Symptoms: Despite prior treatment attempts, symptoms such as pain, swelling, and drainage persist or recur.
- Bone Destruction: Ongoing infection leads to progressive destruction of bone tissue, increasing the risk of complications like fractures or deformities.
- Poor Healing: Wounds associated with chronic osteomyelitis tend to heal slowly or not at all, often requiring advanced wound care interventions.
- Persistent Drainage: Pus or discharge from the wound site may continue despite treatment, indicating ongoing infection.
- Risk of Systemic Spread: If left untreated, chronic osteomyelitis can lead to bloodstream infections or the spread of bacteria to other parts of the body.
Hyperbaric Oxygen Therapy (HBOT) is effective in treating chronic refractory osteomyelitis wounds by delivering high concentrations of oxygen to the affected area, which enhances wound healing. Increased oxygen in the bloodstream greatly enhances the ability of white blood cells to kill bacteria, reduce swelling and allow new blood vessels to grow more rapidly into affected areas including the tissues and bones. This helps to control infection, reduce inflammation, and stimulate tissue repair and regeneration, thus facilitating the healing of stubborn, non-healing osteomyelitis wounds. Typically 20-40 HBOT sessions are required to achieve sustained therapeutic benefit for patients with osteomyelitis.
Osteoradionecrosis wounds are a complication of radiation therapy, typically used in cancer treatment. They primarily affect the bones and surrounding tissues in the irradiated area. Characteristics include:
- Bone Death: Osteoradionecrosis involves the death of bone tissue due to radiation-induced damage to blood vessels, leading to poor blood supply and subsequent tissue decay.
- Non-Healing Wounds: Wounds associated with osteoradionecrosis often fail to heal properly due to compromised blood flow and impaired tissue regeneration.
- Chronic Pain: Patients may experience persistent pain at the site of the affected bone, which can be severe and debilitating.
- Risk Factors: Common risk factors include high radiation doses, repeated radiation treatments, and underlying conditions like diabetes or vascular disease.
- Management: Treatment typically involves a multidisciplinary approach, including medication to manage pain, antibiotics to prevent infection, and, in severe cases, surgical interventions such as debridement or reconstruction. Early detection and management are crucial to prevent progression and complications.
Hyperbaric Oxygen Therapy (HBOT) is effective in treating osteoradionecrosis wounds because it enhances oxygen delivery to damaged tissues, promoting healing and reducing infection risk. Increased oxygen levels stimulate angiogenesis (new blood vessel formation), enhance collagen production, and improve the function of white blood cells, all of which are crucial for tissue repair. Additionally, HBOT reduces tissue edema and helps mitigate the effects of radiation-induced damage, ultimately supporting the regeneration of healthy tissue in osteoradionecrosis wounds.
Soft tissue radionecrosis refers to the death of soft tissues due to exposure to radiation therapy. It typically manifests as a late complication of radiation treatment for cancer. Characteristics of soft tissue radionecrosis include:
- Delayed Onset: Symptoms may arise months to years after radiation therapy, often after the completion of treatment.
- Progressive Tissue Damage: Radiation damages blood vessels, leading to reduced blood supply and subsequent tissue death.
- Non-Healing Ulcers: Ulcers or wounds develop in the affected area and fail to heal properly.
- Pain and Discomfort: Patients may experience persistent pain, swelling, and discomfort at the site of radiation.
- Risk of Infection: The compromised tissue is susceptible to infection, which can exacerbate symptoms and delay healing.
- Impaired Function: Depending on the location and extent of tissue damage, patients may experience limitations in mobility and function.
- Management Challenges: Treatment often involves wound care, pain management, and in severe cases, surgical intervention to remove necrotic tissue. Soft tissue radionecrosis requires careful management and monitoring to prevent complications and optimize patient outcomes.
Hyperbaric Oxygen Therapy (HBOT) is effective in treating Soft Tissue Radionecrosis because it enhances oxygen delivery to damaged tissues, promoting healing and reducing necrosis. By breathing 100% oxygen at high pressure, HBOT increases oxygen concentration in the blood, which helps stimulate the growth of new blood vessels, reduces inflammation, and boosts the body’s natural healing processes. This improved oxygenation supports tissue repair, reduces infection risk, and helps resolve chronic wounds and tissue damage caused by radiation therapy.
Radiation cystitis occurs when capillaries are damaged during radiation treatment and lose the ability to replicate and regrow correctly. This results in telangiectasia and poor tissue perfusion which can lead to both internal and external tissue necrosis.
Key characteristics include:
- Hematuria: Presence of blood in the urine, which may be microscopic or visible.
- Dysuria: Painful or burning sensation during urination.
- Increased Urinary Frequency: Needing to urinate more often than usual.
- Urgency: Sudden, strong urge to urinate.
- Nocturia: Frequent urination during the night.
- Pelvic Pain: Discomfort or pain in the lower abdomen or pelvic area.
- Bladder Irritation: Feeling of bladder fullness or discomfort.
- Urinary Incontinence: Involuntary leakage of urine.
- Chronic Symptoms: Symptoms can persist long after radiation treatment, sometimes becoming long-term.
- Inflammation and Fibrosis: Damage to the bladder’s blood vessels and lining, leading to inflammation and scarring.
Pelvic radiotherapy can cause damage to the tissue and blood vessels in the lining of the bladder. It can cause inflammation and scarring of the bladder lining. This is called radiation cystitis. Radiation cystitis can cause side effects such as blood in the urine (haematuria). This is because radiotherapy can damage the tissue and blood vessels in the lining of the bladder. They can become weaker, and bleed more easily. It can also cause pain or burning when you pass urine (pee) and also make you feel like you need to pass urine frequently.
Randomized studies have shown Hyperbaric Oxygen Therapy (HBOT) to be a valid and effective addition to radiation cystitis treatment plans. It remains the only treatment available that targets and treats inadequate microvasculature, the underlying cause of radiation cystitis. By supporting capillary budding, increasing the vascular epidermal growth factor, and encouraging more normal fibroblast activity, HBOT enables the body to build new granulation tissue with a stronger blood supply and improved oxygenation.
Our Team
With over 20 years of experience and dedication in the wound care space, our team of experts bring passion and insight to every appointment. Our aim is to treat and to heal chronic wounds by uncovering and addressing the root causes, not just treating symptoms. By partnering with your primary physician we create a custom treatment plan to heal your wound quickly.
Contact Us
23838 Valencia Blvd #100,
Valencia, CA 91355
info@scvwoundcare.com
Office Phone
661-425-5000
Fax number
661-200-7201
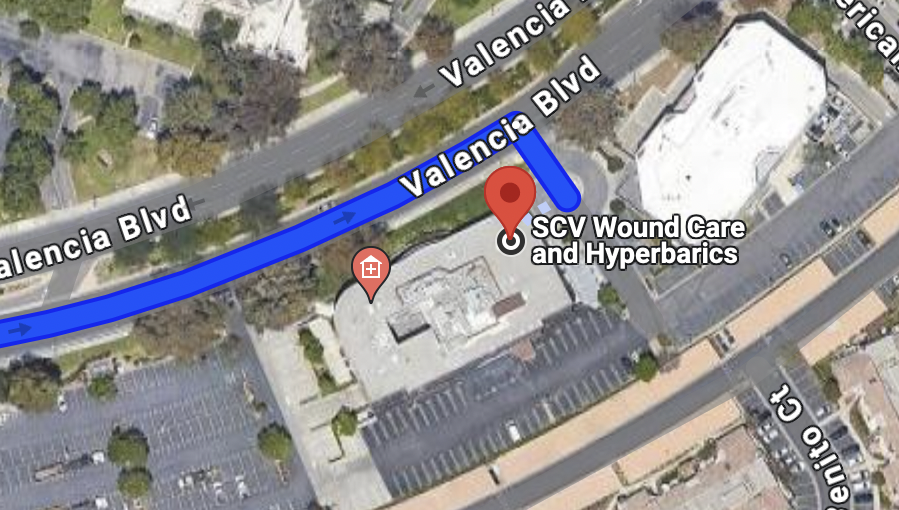
Parking
Our suite entrance is located at the front of the Atrium building. Turn right at the SCV Wound Care and Hyperbarics sign on Valencia Blvd. After turning into the parking, just past the round about, there are three designated parking spots labeled “100” for our suite.
Additional parking and handicap parking available in the parking lot behind the building.